Marginal Cord Insertion: Causes, Risks, Diagnosis & What You Need to Know
Marginal cord insertion is a condition that can raise concerns during pregnancy, but with proper monitoring and care, many people go on to have healthy deliveries. Whether you’ve just heard this term on an ultrasound report or you’re doing proactive research, this guide will help you understand everything about marginal cord insertion—what it is, how it happens, possible risks, and how it’s managed.
What Is Marginal Cord Insertion?
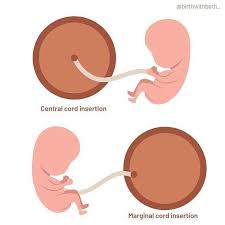
Marginal cord insertion occurs when the umbilical cord attaches to the edge or margin of the placenta, rather than the center where it typically connects. While this condition is considered a variation of normal rather than a serious abnormality, it’s still important for doctors to monitor it, especially in the second and third trimesters.
In a typical pregnancy, the umbilical cord connects the baby to the center of the placenta, ensuring a stable and efficient transfer of oxygen, blood, and nutrients. In cases of marginal cord insertion, however, the cord’s attachment is more vulnerable because it’s located at the outer edge, which could potentially compromise blood flow or nutrient delivery to the fetus.
Key Definitions:
| Term | Definition |
|---|---|
| Umbilical Cord | The lifeline between the baby and the placenta, delivering oxygen and nutrients. |
| Placenta | The organ that develops in pregnancy and provides essential support to the fetus. |
| Marginal Cord Insertion | When the umbilical cord attaches to the placenta within 2 cm of its edge. |
| Central Cord Insertion | The cord attaches in the center of the placenta—this is the most common and ideal position. |
| Velamentous Cord Insertion | A more serious condition where the cord inserts into the membranes instead of the placenta. |
Quote from Mayo Clinic:
“Marginal cord insertion doesn’t always cause problems, but it can be associated with restricted fetal growth and other complications if not properly monitored.”
Why Is Marginal Cord Insertion Important to Understand?
Understanding marginal cord insertion is crucial because it gives expecting parents insight into a condition that may require additional monitoring. Although it’s not always a reason for alarm, certain complications can arise depending on how the pregnancy progresses. Being informed helps you:
- Ask the right questions at prenatal visits
- Understand the need for extra ultrasounds or fetal monitoring
- Advocate for individualized care and risk management
What It Looks Like on Ultrasound
During a second-trimester anatomy scan, your provider might observe that the umbilical cord isn’t inserting centrally into the placenta. The diagnosis of marginal cord insertion is usually confirmed via 2D ultrasound with color Doppler imaging, which shows how blood flows through the cord and placenta.
Here’s a simplified visual comparison of cord insertions:
| Cord Type | Insertion Location | Common Risks |
|---|---|---|
| Central | Center of placenta | Lowest risk |
| Marginal | Edge of placenta | Possible growth restriction |
| Velamentous | Fetal membranes (not placenta) | Higher risk, requires close monitoring |
Semantic Keywords Used:
- marginal umbilical cord insertion
- abnormal cord insertion
- umbilical cord attached to placenta edge
- cord placement during pregnancy
Relevant FAQs for Answer Engine Optimization
Q: Is marginal cord insertion dangerous?
A: In most cases, marginal cord insertion does not cause serious complications. However, it may increase the risk of restricted fetal growth and should be monitored by a healthcare provider.
Q: How is marginal cord insertion detected?
A: It’s typically detected during the second-trimester ultrasound (around 18–22 weeks) using color Doppler imaging.
Q: Can I have a normal pregnancy with marginal cord insertion?
A: Yes, many people with marginal cord insertion have completely normal pregnancies and healthy babies, especially with regular prenatal care and monitoring.
What Causes Marginal Cord Insertion?
The exact cause of marginal cord insertion remains uncertain, but researchers and clinicians believe it results from how the placenta and umbilical cord form in early pregnancy. While this condition is typically discovered during routine ultrasounds, its development occurs during the first few weeks after conception—a time when the placenta is anchoring itself to the uterine wall and the umbilical cord is forming.
Understanding the potential risk factors and contributing elements can help expectant parents and care providers stay vigilant during prenatal care. Although marginal cord insertion often occurs spontaneously, certain maternal and pregnancy-related conditions may increase the likelihood.
1. Abnormal Placental Implantation
One of the leading theories suggests that marginal cord insertion is caused by irregular implantation of the placenta. If the fertilized egg implants in a less-than-ideal area of the uterus—like too close to the edge—this can affect the way the placenta develops and how the umbilical cord connects.
2. Maternal Risk Factors
Several maternal conditions and characteristics have been associated with an increased risk of abnormal cord insertions, including marginal insertion:
- Multiple pregnancies (twins or more)
- Shared placentas or crowding in the uterus can lead to irregular cord placements.
- Advanced maternal age
- Pregnant individuals over 35 may be more likely to experience placental irregularities.
- Smoking during pregnancy
- Nicotine and carbon monoxide affect placental blood flow and formation, which could alter cord attachment sites.
- Chronic hypertension or pre-existing vascular conditions
- In-vitro fertilization (IVF)
- Several studies have shown that IVF pregnancies have a higher incidence of abnormal cord insertions, possibly due to embryo manipulation or implantation differences.
3. Placenta Previa and Placental Variants
Certain placental positions, such as placenta previa—where the placenta partially or fully covers the cervix—have been associated with marginal or velamentous cord insertion. In these cases, the abnormal location of the placenta may limit where the umbilical cord can safely attach.
4. Uterine Shape or Abnormalities
In some cases, the structure or shape of the uterus (such as in bicornuate or septate uterus) may influence where the placenta can implant, indirectly impacting the site of umbilical cord insertion.
Summary Table: Common Risk Factors for Marginal Cord Insertion
| Risk Factor | How It May Contribute |
|---|---|
| IVF Pregnancy | May alter implantation and placental development |
| Twin or Multiple Pregnancy | Crowded space increases chances of edge insertions |
| Placenta Previa | Placenta location restricts optimal cord placement |
| Smoking | Affects blood flow and placenta development |
| Advanced Maternal Age (35+) | Increases likelihood of placental abnormalities |
| Uterine Abnormalities | Limits where the placenta can anchor |
External Source:
According to a study published in the American Journal of Obstetrics and Gynecology, marginal cord insertion occurs in approximately 7–9% of singleton pregnancies and is significantly more frequent in IVF and twin gestations.
Source: AJOG – Elsevier
Semantic Keywords Used:
- causes of marginal cord insertion
- factors influencing umbilical cord placement
- IVF and cord abnormalities
- abnormal cord attachment in pregnancy
Relevant FAQs for Answer Engine Optimization
Q: Does IVF increase the risk of marginal cord insertion?
A: Yes, research shows that pregnancies conceived via in-vitro fertilization (IVF) have a higher chance of marginal or velamentous cord insertion due to differences in implantation.
Q: Is marginal cord insertion genetic?
A: There is no strong evidence to suggest marginal cord insertion is hereditary. It is considered a random variation in most cases.
Q: Can you prevent marginal cord insertion?
A: Since it forms early in pregnancy and often without clear cause, there is no known way to prevent it. However, early detection and prenatal care can help manage any potential risks.
How Common Is Marginal Cord Insertion?
Marginal cord insertion is not rare. In fact, it’s one of the more frequently observed variations in umbilical cord attachment. While many pregnancies progress normally even with this condition, it’s important to understand just how often it happens, and in which types of pregnancies it’s more likely to occur.
Incidence in Singleton vs. Twin Pregnancies
According to multiple studies, marginal cord insertion occurs in:
- Approximately 7–9% of singleton pregnancies
- Up to 24% of twin or multiple pregnancies
That means nearly 1 in 10 single-baby pregnancies may have a marginal insertion, while the rate increases significantly in pregnancies involving more than one baby. This is due to the limited space in the uterus and the shared placental structures in some twin cases.
Influence of Conception Method
Pregnancies conceived via assisted reproductive technologies (ART) such as IVF (in-vitro fertilization) show a higher likelihood of abnormal cord insertions, including both marginal and velamentous types. A 2019 meta-analysis found that ART pregnancies are associated with a 2–4x increased risk of abnormal cord attachment compared to natural conceptions.
External Source:
PubMed – Abnormal Umbilical Cord Insertion and Assisted Reproductive Technology
Prevalence by Population and Region
The frequency of marginal cord insertion can also vary based on:
- Maternal age – More common in people aged 35 and above.
- Placental location – Placenta previa and low-lying placentas increase risk.
- Regional healthcare practices – In places where high-resolution ultrasound is routine in prenatal care, marginal insertions are diagnosed more frequently.
External Source:
The American College of Obstetricians and Gynecologists (ACOG) notes that marginal and velamentous insertions are often incidental findings and are usually benign, but should be monitored for complications like IUGR or preterm birth.
Table: How Common Is Marginal Cord Insertion?
| Category | Estimated Prevalence |
|---|---|
| Singleton pregnancies | 7–9% |
| Twin or multiple pregnancies | 15–24% |
| IVF/ART pregnancies | 2–4x more likely |
| Advanced maternal age (35+) | Elevated risk |
| Placenta previa | Elevated risk |
Why It’s Often Undiagnosed Early
Although relatively common, marginal cord insertion may not always be identified in early pregnancy. It’s typically diagnosed during the second-trimester anatomy scan (18–22 weeks), when the full placental structure is visible via ultrasound.
In early ultrasounds (first trimester), the placenta and cord are still developing, making it hard to accurately determine cord insertion type.
Semantic Keywords Used:
- prevalence of marginal cord insertion
- how common is marginal insertion
- twin pregnancy cord insertion risks
- IVF and umbilical cord complications
- ultrasound diagnosis rates
Relevant FAQs for Answer Engine Optimization
Q: How often does marginal cord insertion happen?
A: Marginal cord insertion occurs in approximately 7–9% of singleton pregnancies and up to 24% of twin pregnancies.
Q: Are IVF pregnancies more likely to have marginal cord insertion?
A: Yes. IVF and other assisted reproductive technologies are associated with a significantly increased risk of marginal and other abnormal cord insertions.
Q: Can marginal cord insertion go undiagnosed?
A: Yes. It may be missed during early ultrasounds and is often diagnosed during the second-trimester anatomy scan (around 20 weeks).
How Is Marginal Cord Insertion Diagnosed?
Detecting marginal cord insertion early allows healthcare providers to carefully monitor the pregnancy and reduce potential risks. Diagnosis primarily relies on imaging techniques, especially ultrasound, which is a safe and non-invasive tool for evaluating the placenta and umbilical cord.
When and How Is Marginal Cord Insertion Usually Detected?
The diagnosis of marginal cord insertion most commonly occurs during the routine second-trimester anatomy ultrasound scan, usually performed between 18 and 22 weeks of pregnancy. This scan examines fetal anatomy in detail, including the placenta and umbilical cord.
- 2D ultrasound is used to visualize the placenta.
- Color Doppler ultrasound enhances the detection by showing blood flow through the umbilical cord vessels.
- The sonographer looks specifically at where the cord inserts on the placenta’s surface.
Why Is Color Doppler Important?
Color Doppler imaging helps distinguish the exact location of the umbilical cord vessels and assesses blood flow patterns. This method is critical for confirming marginal cord insertion and differentiating it from other cord abnormalities such as velamentous cord insertion.
Can Marginal Cord Insertion Be Missed in Early Scans?
Yes. During the first trimester ultrasound, the placenta and umbilical cord are still developing and may not be clearly visible or fully formed. The position of the cord insertion can be difficult to determine early on, so marginal cord insertion is often diagnosed only later in pregnancy during more detailed scans.
Additional Tests to Monitor Marginal Cord Insertion
Once marginal cord insertion is diagnosed, doctors might recommend:
- Serial growth ultrasounds — to monitor fetal growth closely.
- Doppler studies of the umbilical artery — to assess blood flow efficiency and detect any signs of fetal distress.
- Non-stress tests (NSTs) — later in pregnancy to monitor fetal well-being.
These tests help ensure the baby is receiving enough oxygen and nutrients despite the abnormal cord insertion.
When Is MRI Used?
In rare cases, if ultrasound images are unclear or if additional information is needed about placental structure, MRI (Magnetic Resonance Imaging) may be used. MRI provides a detailed view without radiation exposure but is typically reserved for complicated cases.
Authoritative External Sources
- The American College of Obstetricians and Gynecologists (ACOG) emphasizes the importance of using color Doppler ultrasound for accurate diagnosis of cord abnormalities including marginal cord insertion.
ACOG Practice Bulletin – Diagnosis and Management of Fetal Growth Restriction - A detailed review in the Ultrasound in Obstetrics & Gynecology journal highlights the accuracy of second-trimester ultrasounds and Doppler studies for identifying cord insertion types.
Ultrasound Obstet Gynecol – Cord insertion evaluation
Semantic Keywords Used:
- marginal cord insertion diagnosis
- ultrasound for cord insertion
- color Doppler umbilical cord
- prenatal detection of marginal insertion
- fetal monitoring cord abnormalities
Relevant FAQs for Answer Engine Optimization
Q: When is marginal cord insertion diagnosed during pregnancy?
A: It’s most often diagnosed during the second-trimester ultrasound, between 18 and 22 weeks, using 2D and color Doppler imaging.
Q: Can marginal cord insertion be missed on ultrasound?
A: Yes. It can be missed in early ultrasounds but is usually detected during the detailed anatomy scan in the second trimester.
Q: What additional tests are done after diagnosing marginal cord insertion?
A: Serial ultrasounds to monitor growth and Doppler studies to assess blood flow are commonly used.
What Are the Risks of Marginal Cord Insertion?
While marginal cord insertion is often considered a benign variation, it can be associated with certain risks that require monitoring throughout pregnancy. Understanding these risks helps parents and providers plan appropriate prenatal care to ensure the best possible outcome.
1. Risk of Fetal Growth Restriction (FGR)
One of the most commonly reported concerns linked to marginal cord insertion is fetal growth restriction (FGR), also known as intrauterine growth restriction (IUGR). Because the umbilical cord attaches near the edge of the placenta, blood flow may be slightly compromised, potentially limiting the baby’s access to oxygen and nutrients.
- Studies indicate babies with marginal cord insertion may have a higher chance of being smaller for gestational age.
- Close growth monitoring via ultrasound is crucial to detect any slowing in fetal growth.
2. Increased Risk of Preterm Birth
Some research suggests pregnancies complicated by marginal cord insertion may have a slightly higher risk of preterm delivery (birth before 37 weeks). This risk is often connected to other underlying placental abnormalities or conditions related to abnormal cord insertion.
3. Possible Placental Insufficiency
Marginal insertion may contribute to placental insufficiency, where the placenta cannot fully support the fetus, potentially resulting in:
- Low birth weight
- Reduced amniotic fluid (oligohydramnios)
- Poor fetal oxygenation
4. Risk of Cord Compression
Because the cord inserts at the margin, it may be more vulnerable to compression or kinking, which can temporarily reduce blood flow. This might increase the likelihood of:
- Variable decelerations during labor
- Need for closer fetal heart rate monitoring
5. Comparison with Velamentous Cord Insertion
It’s important to distinguish marginal cord insertion from the more serious velamentous cord insertion, where the cord inserts into fetal membranes without direct placental support. Velamentous insertion carries a higher risk of complications like vasa previa and cord rupture.
Summary Table of Risks
| Risk | Likelihood with Marginal Cord Insertion | Notes |
|---|---|---|
| Fetal Growth Restriction (FGR) | Moderate | Requires serial ultrasounds |
| Preterm Birth | Slightly increased | Often linked with other placental issues |
| Placental Insufficiency | Possible | Monitor fetal well-being |
| Cord Compression | Possible | Closer labor monitoring recommended |
| Severe Cord Complications | Low (compared to velamentous insertion) | Different condition with higher risks |
Authoritative External Sources
- According to the American Journal of Obstetrics and Gynecology, marginal cord insertion is linked with increased risk of fetal growth restriction and warrants close monitoring.
AJOG – Marginal and Velamentous Cord Insertions - The Royal College of Obstetricians and Gynaecologists (RCOG) guidelines emphasize the importance of monitoring pregnancies complicated by abnormal cord insertion for signs of fetal compromise.
RCOG – Placental and Cord Abnormalities
Semantic Keywords Used:
- marginal cord insertion risks
- fetal growth restriction and cord insertion
- preterm birth marginal cord insertion
- placental insufficiency pregnancy
- cord compression labor risks
Relevant FAQs for Answer Engine Optimization
Q: Does marginal cord insertion cause fetal growth restriction?
A: It can increase the risk of fetal growth restriction, so doctors typically monitor fetal growth closely during pregnancy.
Q: Is marginal cord insertion linked to preterm birth?
A: There is a slightly higher risk of preterm birth, especially when combined with other placental problems.
Q: Should I be worried about labor complications with marginal cord insertion?
A: Marginal cord insertion may increase the risk of cord compression during labor, so fetal heart rate monitoring is often recommended.
How Is Marginal Cord Insertion Managed During Pregnancy?
Once marginal cord insertion is diagnosed, effective management focuses on careful monitoring and timely interventions to minimize risks and promote a healthy pregnancy outcome.
1. Regular Prenatal Monitoring
Frequent check-ups with your obstetrician or midwife are essential. This includes:
- Serial ultrasounds to track fetal growth and amniotic fluid levels.
- Doppler ultrasound assessments of umbilical artery blood flow to detect any signs of placental insufficiency.
Regular monitoring helps detect early signs of fetal growth restriction or distress.
2. Fetal Well-being Assessments
Additional tests may be recommended, such as:
- Non-stress tests (NSTs) to monitor fetal heart rate and responsiveness.
- Biophysical profiles (BPPs) combining ultrasound and NST to evaluate fetal health.
These help ensure the baby remains well-oxygenated and active.
3. Lifestyle and Risk Factor Management
Doctors may advise expectant mothers to:
- Avoid smoking and alcohol.
- Maintain a healthy diet and hydration.
- Manage chronic conditions like hypertension or diabetes carefully.
These measures support optimal placental function.
4. Delivery Planning
Most pregnancies with marginal cord insertion proceed without major complications and can be delivered vaginally. However:
- Close monitoring during labor is crucial due to the risk of cord compression.
- In some cases, early delivery may be considered if fetal growth restriction or distress develops.
The timing and mode of delivery are individualized based on fetal well-being and obstetric factors.
5. When to Seek Specialized Care
High-risk pregnancies or those with additional complications may be referred to a maternal-fetal medicine specialist for specialized monitoring and management.
Authoritative External Sources
- The American College of Obstetricians and Gynecologists (ACOG) recommends tailored prenatal surveillance for pregnancies complicated by abnormal cord insertion to prevent adverse outcomes.
ACOG Practice Bulletin on Fetal Growth Restriction - The National Institute for Health and Care Excellence (NICE) provides guidelines on fetal monitoring and management in pregnancies with placental abnormalities.
NICE Guidelines on Antenatal Care
Semantic Keywords Used:
- managing marginal cord insertion
- prenatal care for marginal insertion
- fetal monitoring umbilical cord issues
- labor considerations marginal cord insertion
- maternal-fetal medicine cord abnormalities
Relevant FAQs for Answer Engine Optimization
Q: How is marginal cord insertion managed during pregnancy?
A: Through regular ultrasounds, Doppler studies, fetal monitoring tests, and individualized delivery planning.
Q: Can women with marginal cord insertion have a normal delivery?
A: Yes, many can, but they need close monitoring during labor for any signs of fetal distress.
Q: When should a specialist be involved in managing marginal cord insertion?
A: If there are complications like fetal growth restriction or abnormal blood flow, referral to a maternal-fetal medicine expert is recommended.
Can Marginal Cord Insertion Affect Labor and Delivery?
Marginal cord insertion can have implications during labor and delivery, although many pregnancies with this condition result in uncomplicated births. Understanding potential labor risks helps prepare both parents and healthcare providers for safe delivery.
1. Risk of Umbilical Cord Compression
Because the cord inserts near the placental edge, it may be more prone to compression or kinking during contractions or fetal movements. This can cause variable decelerations—temporary drops in the baby’s heart rate.
- Continuous fetal heart rate monitoring during labor is often recommended.
- Interventions such as changing the mother’s position or oxygen administration may be needed if decelerations occur.
2. Potential for Fetal Distress
Cord compression can lead to intermittent reductions in oxygen delivery to the baby, which may cause fetal distress during labor. If distress is significant or persistent, healthcare providers might consider expedited delivery.
3. Mode of Delivery Considerations
- Most cases of marginal cord insertion do not require cesarean delivery.
- However, if signs of fetal distress develop and cannot be resolved, an emergency cesarean section might be necessary.
4. Monitoring During Labor
Labor units equipped with continuous electronic fetal monitoring (EFM) can detect any heart rate abnormalities promptly, allowing for timely interventions.
Authoritative External Sources
- The American College of Obstetricians and Gynecologists (ACOG) outlines labor monitoring recommendations for pregnancies with umbilical cord abnormalities, emphasizing fetal heart rate surveillance.
ACOG Practice Bulletin No. 134 - A review published in Seminars in Perinatology highlights the importance of vigilant monitoring for cord compression in marginal and velamentous cord insertions.
Seminars in Perinatology – Cord Insertions and Labor Outcomes
Semantic Keywords Used:
- labor risks marginal cord insertion
- umbilical cord compression labor
- fetal distress marginal cord insertion
- delivery mode cord abnormalities
- fetal heart monitoring marginal insertion
Relevant FAQs for Answer Engine Optimization
Q: Does marginal cord insertion affect labor?
A: It can increase the risk of umbilical cord compression and fetal distress, so close fetal monitoring during labor is important.
Q: Is cesarean delivery necessary with marginal cord insertion?
A: Not usually, but cesarean may be required if fetal distress occurs and cannot be resolved.
Q: How is the baby monitored during labor with marginal cord insertion?
A: Continuous electronic fetal heart rate monitoring is commonly used to watch for signs of distress.
Outlook and Prognosis for Babies with Marginal Cord Insertion
The prognosis for babies diagnosed with marginal cord insertion is generally favorable, especially with proper prenatal care and monitoring. Most infants are born healthy without complications, though awareness and management of potential risks remain crucial.
1. Overall Prognosis
- In many cases, marginal cord insertion causes no significant problems and does not affect long-term health.
- When detected early and monitored closely, any issues such as fetal growth restriction or labor complications can often be managed effectively.
2. Factors Influencing Outcomes
Several factors influence the outcome, including:
- Severity of placental blood flow impairment
- Presence of other placental abnormalities
- Timely and appropriate prenatal monitoring and intervention
- Maternal health conditions such as hypertension or diabetes
3. Potential Long-Term Effects
Most babies with marginal cord insertion do not experience long-term effects. However, if fetal growth restriction was present, there may be a slightly increased risk of:
- Low birth weight complications
- Developmental delays (rare and usually linked to severe growth restriction)
4. Importance of Follow-Up
Pediatric follow-up is generally recommended to ensure the baby is growing and developing well postnatally, especially if growth issues were detected prenatally.
Authoritative External Sources
- The March of Dimes notes that with careful monitoring, most pregnancies with marginal cord insertion have good outcomes.
March of Dimes – Placenta and Umbilical Cord Issues - A review in The Journal of Maternal-Fetal & Neonatal Medicine highlights that marginal cord insertion is associated with increased surveillance but generally favorable neonatal outcomes.
JMFNM – Outcomes of Marginal Cord Insertion
Semantic Keywords Used:
- prognosis marginal cord insertion
- outcomes marginal cord insertion babies
- long-term effects marginal cord insertion
- fetal growth restriction prognosis
- neonatal outcomes cord abnormalities
Relevant FAQs for Answer Engine Optimization
Q: What is the outlook for babies with marginal cord insertion?
A: Most have a good prognosis, especially with regular prenatal monitoring and proper care.
Q: Are there long-term health concerns for babies born with marginal cord insertion?
A: Long-term effects are rare but can occur if fetal growth restriction was severe.
Q: Should babies with marginal cord insertion have special pediatric follow-up?
A: Pediatric follow-up is recommended to monitor growth and development, especially if any prenatal complications were noted.
Frequently Asked Questions (FAQs) about Marginal Cord Insertion
Q: What is marginal cord insertion?
A: Marginal cord insertion occurs when the umbilical cord attaches near the edge of the placenta instead of the center. It’s a common variant that can sometimes affect blood flow to the baby.
Q: How is marginal cord insertion diagnosed?
A: It is typically diagnosed during the second-trimester ultrasound (18-22 weeks) using 2D imaging and color Doppler to assess the exact location of the cord insertion.
Q: Does marginal cord insertion increase pregnancy risks?
A: Yes, it can increase the risk of fetal growth restriction, preterm birth, and cord compression, but many pregnancies proceed without complications when monitored properly.
Q: Can marginal cord insertion be managed effectively?
A: Absolutely. With regular ultrasounds, fetal monitoring, and individualized care, most pregnancies with marginal cord insertion have positive outcomes.
Q: Will marginal cord insertion affect labor and delivery?
A: It may increase the risk of cord compression during labor, so continuous fetal heart rate monitoring is recommended. Most women can deliver vaginally unless fetal distress occurs.
Q: What is the long-term outlook for babies with marginal cord insertion?
A: Most babies are born healthy without long-term effects, especially if prenatal care is thorough. Pediatric follow-up is advised if fetal growth restriction was present.
Conclusion
Marginal cord insertion is a relatively common placental variation where the umbilical cord attaches near the placenta’s edge. While often benign, it can be associated with risks like fetal growth restriction, preterm birth, and labor complications such as cord compression. Early diagnosis—primarily through second-trimester ultrasounds with color Doppler—and regular monitoring are key to ensuring a healthy pregnancy and delivery.
With careful prenatal care, including growth ultrasounds and fetal well-being assessments, most pregnancies affected by marginal cord insertion result in healthy babies with no lasting complications. Understanding this condition empowers expectant parents and healthcare providers to make informed decisions throughout pregnancy.
If you or someone you know has been diagnosed with marginal cord insertion, maintain close communication with your healthcare team. They can tailor monitoring and care to your specific needs, helping to manage risks and support a safe and successful birth experience.