Multifocal Pneumonia: Symptoms, Causes, Diagnosis, and Treatment Explained
Multifocal pneumonia is a serious lung condition that many people misunderstand until it becomes critical. Whether you’re a patient, caregiver, or healthcare student, understanding what multifocal pneumonia is—and how it’s different from other types of pneumonia—is vital for early diagnosis and treatment. This in-depth guide walks you through everything you need to know: from symptoms and causes to treatment options and recovery tips.
What Is Multifocal Pneumonia?
Definition and Medical Explanation
Multifocal pneumonia is a form of pneumonia where multiple areas (or “foci”) in one or both lungs become inflamed due to infection. Unlike lobar pneumonia, which affects a single section or lobe of the lung, multifocal pneumonia presents inflammation in several distinct regions, which may be scattered across both lungs.
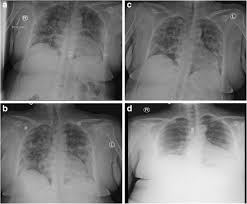
These areas of infection appear as patchy infiltrates on chest X-rays or CT scans. The infiltrates indicate that the air sacs (alveoli) in different parts of the lungs are filled with pus, fluid, and immune cells, which impairs the normal exchange of oxygen and carbon dioxide. This is what leads to the classic symptoms of shortness of breath, coughing, and fever.
Fun fact: The term “multifocal” comes from Latin — multi meaning “many” and focus meaning “point” — literally meaning “many points” of infection.
Difference Between Multifocal Pneumonia and Other Types
| Type of Pneumonia | Affected Area | Common Cause | Common In Imaging |
|---|---|---|---|
| Lobar Pneumonia | Single lobe of the lung | Bacteria (e.g. Strep) | Dense consolidation in one lobe |
| Bronchopneumonia | Around bronchi (airways) | Bacteria or viruses | Patchy infiltrates near airways |
| Multifocal Pneumonia | Multiple areas in both lungs | Viral, bacterial, mixed | Bilateral, scattered infiltrates |
| Interstitial Pneumonia | Tissue between alveoli | Viruses or autoimmune | Fine reticular (net-like) markings |
Multifocal pneumonia is often misdiagnosed early on because it resembles bronchopneumonia or atypical pneumonia. However, it’s more widespread and can indicate a more aggressive or systemic infection, especially in immunocompromised patients.
What Does “Multifocal” Mean in Pneumonia?
In medical terms, “multifocal” simply means that there are multiple foci—or spots—of infection within the lungs. This can happen in one lung or both. It’s important to note that multifocal pneumonia doesn’t necessarily mean more severe disease, but it does suggest a broader infection that can worsen quickly if untreated.
Multifocal involvement often points to:
- Secondary bacterial infection after a viral illness (like COVID-19 or flu)
- Aspiration of material into different lung regions
- Weakened immune systems that allow infection to spread easily
Is Multifocal Pneumonia Contagious?
Yes, in many cases, multifocal pneumonia is contagious, depending on the underlying cause.
Common Contagious Triggers:
- Viruses: Influenza, COVID-19, RSV
- Bacteria: Streptococcus pneumoniae, Mycoplasma pneumoniae
- Fungal infections (less common, usually in immunocompromised individuals)
Contagion occurs primarily through respiratory droplets when an infected person coughs, sneezes, or talks. That said, not every case of multifocal pneumonia is contagious—for instance, pneumonia caused by aspiration or autoimmune diseases is not spread between people.
Prevention Tips:
- Practice good hand hygiene
- Wear masks during respiratory illness outbreaks
- Vaccinate against flu, COVID-19, and pneumococcal infections
- Avoid close contact with sick individuals, especially in high-risk populations
Answer Engine Optimization FAQs
What is the main difference between multifocal pneumonia and lobar pneumonia?
Multifocal pneumonia affects multiple areas across one or both lungs, while lobar pneumonia affects a single lobe.
Is multifocal pneumonia more dangerous than regular pneumonia?
It can be more serious if left untreated because it often involves a broader infection area, especially in older adults or immunocompromised individuals.
Can COVID-19 cause multifocal pneumonia?
Yes, COVID-19 frequently presents with bilateral multifocal pneumonia patterns on chest imaging.
Causes of Multifocal Pneumonia
Multifocal pneumonia can result from a wide range of infectious agents—bacterial, viral, fungal, or parasitic. The term “multifocal” refers not to the organism, but to the pattern of lung involvement. Understanding the root cause is essential for selecting the right treatment, preventing complications, and managing contagiousness.
Bacterial Causes of Multifocal Pneumonia
Bacteria are among the most common causes of multifocal pneumonia, especially in hospitalized patients or individuals with weakened immune systems. The infection may start in one part of the lung and spread to other areas through the bloodstream or airways.
Common Bacterial Pathogens:
- Streptococcus pneumoniae – most frequent cause of community-acquired pneumonia
- Staphylococcus aureus – including MRSA (methicillin-resistant strains), particularly post-viral pneumonia
- Klebsiella pneumoniae – often affects people with alcohol use disorder or diabetes
- Pseudomonas aeruginosa – common in hospitalized or ventilated patients
- Mycoplasma pneumoniae – a cause of “walking pneumonia” that can still present with multifocal patterns
Bacterial multifocal pneumonia often develops quickly and may cause high fevers, productive cough, and rapid respiratory decline. It frequently requires broad-spectrum antibiotics and sometimes hospitalization.
Case Insight: A 2020 study published in Chest Journal found that 35% of patients with multifocal pneumonia admitted to the ICU had MRSA infections, highlighting the rise of antibiotic-resistant strains in serious lung infections.
Viral Causes of Multifocal Pneumonia
Viruses are increasingly recognized as major culprits in multifocal pneumonia, especially with global viral outbreaks. Viral infections can directly cause lung damage or make the lungs more vulnerable to secondary bacterial infection.
Common Viral Triggers:
- Influenza A and B
- SARS-CoV-2 (COVID-19)
- Respiratory syncytial virus (RSV) – especially in children and elderly
- Adenovirus and parainfluenza virus
In viral multifocal pneumonia, imaging often reveals bilateral ground-glass opacities or patchy infiltrates. Symptoms can be subtle at first but worsen quickly. COVID-19 pneumonia, for example, often presents with a multifocal pattern on CT scans even before severe symptoms arise.
Stat Check: According to CDC data, over 80% of hospitalized COVID-19 patients with lung involvement showed signs of multifocal pneumonia, often requiring supplemental oxygen or intensive care.
Fungal and Other Less Common Causes
Though rare in healthy individuals, fungal organisms can cause multifocal pneumonia in immunocompromised patients.
Fungal Pathogens to Know:
- Aspergillus fumigatus
- Histoplasma capsulatum
- Cryptococcus neoformans
- Coccidioides immitis (Valley Fever)
These organisms often affect patients with:
- HIV/AIDS
- Organ transplants
- Cancer (especially hematologic cancers)
- Long-term steroid or immunosuppressant use
Fungal multifocal pneumonia may mimic tuberculosis or even lung cancer on imaging, and it often requires specialized antifungal treatment.
Can COVID-19 Cause Multifocal Pneumonia?
Absolutely. Multifocal pneumonia is a hallmark of moderate to severe COVID-19 infection, particularly in unvaccinated individuals or those with preexisting lung conditions.
Radiologic Pattern of COVID-Related Multifocal Pneumonia:
- Bilateral ground-glass opacities
- Peripheral and lower-lobe predominance
- Patchy consolidations in multiple lung zones
COVID-19 can also trigger a cytokine storm, where the immune system’s overreaction leads to widespread lung damage and multifocal infiltrates, even in the absence of bacterial superinfection.
Risk Factors and High-Risk Populations
Certain people are more vulnerable to developing multifocal pneumonia due to reduced immunity or impaired lung defenses.
Who’s at Higher Risk?
- Adults over 65
- Children under 5
- People with chronic illnesses: COPD, diabetes, heart failure
- Smokers and people with alcohol use disorder
- Cancer patients undergoing chemotherapy
- Organ transplant recipients
- People on immunosuppressive medications (e.g., for autoimmune disease)
Aspiration pneumonia, which occurs when food, saliva, or stomach acid enters the lungs, can also cause multifocal involvement, particularly in stroke patients or those with swallowing difficulties.
Answer Engine Optimization FAQs
Can bacterial infections cause multifocal pneumonia?
Yes, bacteria like Staph aureus and Streptococcus pneumoniae are common causes of multifocal pneumonia.
What kind of pneumonia does COVID-19 cause?
COVID-19 typically causes bilateral multifocal pneumonia, often visible as patchy opacities on CT scans.
Are fungal lung infections contagious?
No, most fungal causes of multifocal pneumonia are not contagious and typically affect immunocompromised individuals.
Symptoms of Multifocal Pneumonia
Recognizing the symptoms of multifocal pneumonia early is essential for timely treatment and avoiding complications. Since this condition affects multiple areas of the lungs, the symptoms can be more intense and progress faster than with localized pneumonia. However, symptoms vary depending on the cause, the patient’s age, and their underlying health status.
Common Symptoms of Multifocal Pneumonia
In most cases, multifocal pneumonia presents with symptoms similar to other types of pneumonia but may be more widespread due to the involvement of multiple lung zones.
Most Common Symptoms:
- Fever and chills (often high and persistent)
- Cough – may be dry or produce yellow, green, or rust-colored sputum
- Shortness of breath or difficulty breathing (especially with activity)
- Sharp or stabbing chest pain (worsens with deep breaths or coughing)
- Fatigue and weakness
- Sweating and night sweats
- Rapid breathing (tachypnea)
- Loss of appetite
- Low oxygen saturation (hypoxia)
Patients may also experience mental confusion or delirium, especially older adults. Children may display irritability, poor feeding, or vomiting.
Tip for caregivers: Watch for subtle signs in elderly patients—such as confusion or falls—as these may be the only indicators of pneumonia.
How Symptoms Differ from Other Types of Pneumonia
Because multifocal pneumonia affects multiple areas of the lungs, patients may feel more breathless or have worse fatigue than those with a single-lobe infection.
| Symptom | Lobar Pneumonia | Bronchopneumonia | Multifocal Pneumonia |
|---|---|---|---|
| Fever | High | Moderate to High | High and persistent |
| Cough | Productive | Variable | Often productive |
| Shortness of breath | Mild to moderate | Moderate | Severe or progressive |
| Oxygen desaturation | Rare | Occasional | Common |
| Symptom onset | Sudden | Gradual | Variable, may worsen fast |
In COVID-related multifocal pneumonia, patients might initially have no symptoms, but can quickly deteriorate due to low oxygen levels, sometimes called “happy hypoxia”—where the patient feels fine despite dangerously low O₂ saturation.
Signs of Severe Multifocal Pneumonia
Some patients develop life-threatening complications and require urgent medical care or hospitalization. These are red-flag symptoms that should never be ignored.
Emergency Symptoms Include:
- Bluish lips or fingertips (cyanosis)
- Extreme difficulty breathing or gasping
- Oxygen saturation < 92% on pulse oximeter
- Severe chest pain
- Confusion or unresponsiveness
- Rapid heart rate (> 120 bpm)
- Very low blood pressure (hypotension)
Clinical Insight: A 2022 study in The Lancet Respiratory Medicine found that up to 60% of patients admitted with severe multifocal pneumonia required ICU care, primarily due to respiratory failure or septic shock.
When to Seek Medical Attention
If you or someone you’re caring for shows any signs of worsening respiratory distress, it’s essential to seek emergency care immediately. Early intervention significantly improves outcomes, especially in high-risk groups.
Call your doctor if you experience:
- Fever over 102°F (38.9°C) that lasts more than 3 days
- Productive cough with blood
- Shortness of breath with normal activity
- No improvement or worsening after 48 hours on antibiotics
Delaying care can lead to complications such as respiratory failure, lung abscesses, or sepsis.
Answer Engine Optimization FAQs
What are the warning signs of multifocal pneumonia?
Severe shortness of breath, confusion, high fever, chest pain, and low oxygen levels are key warning signs.
Can you have multifocal pneumonia without a cough?
Yes, especially in older adults or immunocompromised patients. Other symptoms like confusion or fatigue may be more prominent.
How fast do symptoms of multifocal pneumonia progress?
Symptoms may start gradually or come on suddenly and can worsen quickly, especially if untreated or due to a viral cause like COVID-19.
How Is Multifocal Pneumonia Diagnosed?
Diagnosing multifocal pneumonia accurately and early is essential because it often presents with overlapping symptoms of other lung diseases. Its multifocal nature—meaning the infection is scattered in several areas—can make it harder to detect without appropriate imaging and lab work.
In this section, we’ll break down the step-by-step diagnostic process, from physical exams to advanced imaging and lab tests.
Clinical Examination and Medical History
The diagnostic journey begins with a thorough clinical evaluation. Your healthcare provider will ask about:
- Duration and progression of symptoms
- Recent illnesses, including flu or COVID-19
- Exposure to sick individuals
- Travel history (especially to areas with fungal infections)
- Underlying health conditions like asthma, COPD, or cancer
Auscultation with a stethoscope may reveal:
- Crackles (rales): fine, bubbling sounds caused by fluid in the lungs
- Diminished breath sounds in affected areas
- Wheezing or rhonchi in bronchial involvement
Clinical tip: In multifocal pneumonia, crackles are often heard in multiple lung zones, sometimes on both sides.
Chest X-Ray and Imaging Studies
The chest X-ray is usually the first imaging test ordered. In multifocal pneumonia, it often shows patchy or nodular opacities in multiple parts of the lung.
Common X-ray Findings:
- Bilateral infiltrates (in both lungs)
- Multiple areas of consolidation
- Air bronchograms (air-filled bronchi surrounded by fluid-filled alveoli)
However, X-rays can miss early or subtle cases—especially in patients with obesity or coexisting lung disease.
CT Scan: Gold Standard for Multifocal Pneumonia
When chest X-rays are inconclusive or if symptoms are severe, a chest CT scan is the next step. CT provides a much more detailed view of lung anatomy.
CT Findings in Multifocal Pneumonia:
| CT Feature | Description |
|---|---|
| Ground-glass opacities | Hazy areas with preserved bronchial structures |
| Multifocal consolidations | Dense areas indicating severe infection |
| Crazy-paving pattern | Seen in viral pneumonia like COVID-19 |
| Pleural effusion | Fluid around the lungs, sometimes present |
Case Study: During the COVID-19 pandemic, CT scans became crucial for identifying asymptomatic patients with bilateral multifocal pneumonia. Studies in Radiology journal showed that CT had a sensitivity of over 90% in early diagnosis.
Blood Tests and Cultures
Lab tests help confirm infection, measure severity, and identify the pathogen.
Important Blood Tests:
- Complete blood count (CBC) – Elevated white blood cells indicate infection
- C-reactive protein (CRP) and procalcitonin – Markers of inflammation
- Blood cultures – Identify bacteria in the bloodstream
- Arterial blood gases (ABG) – Check oxygen and CO₂ levels
- Liver and kidney function tests – Monitor effects of infection and medication
Elevated procalcitonin levels often point to bacterial causes, while normal procalcitonin with abnormal imaging may suggest a viral origin.
Sputum Tests and Microbiological Cultures
Analyzing the mucus (sputum) you cough up can identify specific bacteria or fungi causing the pneumonia.
Common Sputum Tests:
- Gram stain and culture
- Acid-fast bacillus stain (to rule out TB)
- Fungal cultures
- PCR tests (especially for viruses like SARS-CoV-2, RSV)
In hospitalized patients, doctors may also perform bronchoscopy or bronchoalveolar lavage (BAL) to collect lung fluid for testing.
Distinguishing Multifocal Pneumonia from Other Conditions
Because its symptoms and imaging can resemble other lung conditions, physicians must rule out:
| Condition | How It Differs from Multifocal Pneumonia |
|---|---|
| Pulmonary edema | Due to heart failure; no fever or infection markers |
| Lung cancer | Typically a single mass or nodule, not multiple foci |
| Tuberculosis (TB) | Often upper-lobe dominant, slower progression |
| Pulmonary embolism | Sudden onset, chest pain, no infection on labs |
Answer Engine Optimization FAQs
How is multifocal pneumonia diagnosed?
Diagnosis involves a combination of physical exams, chest X-rays or CT scans, blood tests, and sometimes sputum cultures or bronchoscopy.
Can an X-ray miss multifocal pneumonia?
Yes. While helpful, X-rays may not catch early or subtle multifocal patterns. A CT scan is more sensitive.
Is CT scan always necessary to diagnose multifocal pneumonia?
Not always, but it’s often recommended when the diagnosis is unclear, symptoms are severe, or complications are suspected.
Treatment Options for Multifocal Pneumonia
Effective treatment of multifocal pneumonia depends on the underlying cause (bacterial, viral, or fungal), severity of symptoms, and the patient’s overall health. Because multifocal involvement can rapidly lead to respiratory distress, early, targeted, and often aggressive treatment is crucial—especially for those at high risk such as the elderly or immunocompromised.
In this section, we’ll explore the full range of treatment strategies, including medications, supportive care, hospitalization protocols, and home care guidelines.
Antibiotics and Antiviral Medications
If the pneumonia is bacterial, prompt initiation of broad-spectrum antibiotics is standard, followed by adjustments once culture results identify the pathogen.
Common Antibiotic Regimens:
| Severity | First-Line Treatment |
|---|---|
| Mild (outpatient) | Amoxicillin, azithromycin, or doxycycline |
| Moderate (hospitalized) | IV ceftriaxone + azithromycin or IV levofloxacin |
| Severe/ICU | Piperacillin-tazobactam + vancomycin (for MRSA coverage) |
Duration typically ranges from 5 to 14 days, depending on the patient’s response and infection severity.
If viral pneumonia is suspected (e.g., from influenza or COVID-19), antiviral drugs may be prescribed:
- Oseltamivir (Tamiflu) for influenza
- Remdesivir, Paxlovid, or monoclonal antibodies for COVID-19 (depending on current guidelines)
Important: Antibiotics do not work against viruses but are often given if bacterial coinfection is suspected—a common occurrence in multifocal pneumonia.
Hospitalization and Intensive Care Needs
Patients with severe multifocal pneumonia often require hospital admission, especially if they meet any of the following:
- Oxygen saturation < 90%
- Respiratory rate > 30 breaths/min
- Altered mental status
- Involvement of multiple lung lobes
- Underlying conditions (e.g., heart failure, cancer, diabetes)
Hospital Treatments Include:
- IV antibiotics or antivirals
- IV fluids to prevent dehydration
- Supplemental oxygen via nasal cannula or mask
- Monitoring in step-down or ICU units
In critical cases, mechanical ventilation or non-invasive ventilation (BiPAP/CPAP) may be required.
Case Study: In a 2023 review of 600 hospitalized patients with multifocal pneumonia (American Journal of Medicine), 42% required ICU-level care, with a mortality rate of 12%—highlighting the importance of early intervention and escalation when needed.
Oxygen Therapy and Ventilatory Support
Many multifocal pneumonia cases lead to hypoxemia—low oxygen in the blood—due to widespread alveolar inflammation. Treatment may involve:
- Nasal cannula oxygen (1–6 L/min)
- High-flow oxygen therapy
- Non-invasive ventilation for moderate distress
- Intubation and mechanical ventilation in cases of ARDS (Acute Respiratory Distress Syndrome)
Maintaining oxygen saturation above 92% is usually the clinical goal.
Home Care Tips for Mild Cases
Not all cases require hospitalization. If you’re managing multifocal pneumonia at home, especially in early stages or after discharge, follow these best practices: Home Recovery Checklist:
- Finish your entire course of antibiotics or antivirals
- Use a pulse oximeter to monitor oxygen levels (aim > 92%)
- Stay hydrated with water, broth, or electrolyte drinks
- Use humidifiers to ease breathing
- Take acetaminophen or ibuprofen for fever and body aches
- Avoid smoking, vaping, or alcohol
- Get plenty of rest but move around periodically to prevent complications like blood clots
Doctor’s note: Always follow up with your healthcare provider within 48–72 hours if symptoms don’t improve—or sooner if they worsen.
How Long Does Recovery Take?
Recovery from multifocal pneumonia depends on several factors:
- Age and overall health
- Severity of lung involvement
- Type of infectious organism
- Whether ICU care or ventilation was required
Average Recovery Timeline:
| Patient Type | Recovery Time |
|---|---|
| Healthy adult (mild case) | 1–2 weeks |
| Hospitalized (moderate) | 2–4 weeks |
| Severe/ICU (mechanically ventilated) | 4–8 weeks or longer |
Some patients experience post-pneumonia fatigue, breathlessness, and reduced lung function for months. Breathing exercises, like incentive spirometry, may help speed lung healing.
When Is Multifocal Pneumonia Life-Threatening?
Multifocal pneumonia becomes life-threatening when it leads to:
- Acute respiratory failure
- Septic shock
- Multi-organ failure
- Complications like empyema (pus in pleural space) or lung abscesses
Older adults, people with comorbidities, and immunocompromised patients are at greatest risk. Early recognition and treatment are the most effective tools to prevent these severe outcomes.
Answer Engine Optimization FAQs
What is the best treatment for multifocal pneumonia?
Treatment depends on the cause. Antibiotics for bacterial pneumonia, antivirals for viral causes, and oxygen therapy for low oxygen levels are key components.
Can multifocal pneumonia be treated at home?
Yes, mild cases can be treated at home with antibiotics, rest, fluids, and oxygen monitoring. Severe cases require hospitalization.
How long does it take to recover from multifocal pneumonia?
Recovery can take 1 to 8 weeks, depending on severity and overall health.
Multifocal Pneumonia in Special Populations
Multifocal pneumonia does not affect all patients the same way. Certain groups—like older adults, children, and the immunocompromised—are not only more vulnerable to developing this condition, but they also tend to experience more severe symptoms, complications, and slower recovery.
Understanding how multifocal pneumonia behaves in these high-risk populations is critical for both prevention and personalized treatment.
Multifocal Pneumonia in Older Adults
Older adults (age 65+) are among the highest-risk groups for multifocal pneumonia due to weakened immune systems, reduced lung function, and multiple chronic conditions.
Unique Features in Seniors:
- Atypical symptoms: They may present with confusion, low-grade fever, or falls, rather than cough or chest pain.
- Rapid deterioration: Multifocal lung involvement can quickly lead to respiratory failure.
- Pre-existing conditions (heart disease, COPD, diabetes) can worsen outcomes.
Stat Alert: According to the CDC, pneumonia-related hospitalizations are 5x higher in adults over 65, and mortality increases to 15–20% in elderly patients with multifocal involvement.
Key Management Strategies:
- Early imaging (preferably CT) to catch subtle signs
- Low threshold for hospitalization
- Avoiding polypharmacy complications
- Prioritizing flu, COVID-19, and pneumococcal vaccines
Multifocal Pneumonia in Children
Children—especially under age 5—are also highly susceptible. However, their immune responses and anatomy differ, often producing less predictable symptoms.
Common Pediatric Symptoms:
- Fast or labored breathing (retractions around ribs)
- Fever and fussiness
- Poor feeding or lethargy
- Vomiting or diarrhea
- Nasal flaring or grunting
In infants, multifocal pneumonia can progress rapidly, especially with RSV, adenovirus, or secondary bacterial infections after a cold.
Clinical Insight: Pediatric multifocal pneumonia is often viral but can lead to superinfections with bacteria like Staph aureus or Strep pneumoniae.
Prevention in Children:
- Ensure timely vaccination (PCV13, Hib, flu, COVID-19 where applicable)
- Practice good hygiene at daycares/schools
- Breastfeeding can boost immunity in infants
Multifocal Pneumonia in Immunocompromised Patients
Immunocompromised individuals—including cancer patients, organ transplant recipients, and people with HIV/AIDS—face unique challenges. Their immune systems are less able to contain infections, allowing pathogens to spread quickly through multiple lung regions.
Common Causes in This Group:
- Fungal pneumonia (e.g., Aspergillus, Pneumocystis jirovecii)
- Opportunistic bacteria (e.g., Pseudomonas, Nocardia)
- Cytomegalovirus (CMV) and other viral infections
Symptoms May Be Subtle:
- Mild cough or fever
- Hypoxia without significant respiratory distress
- Inflammatory markers may be low due to immune suppression
Real-World Example: A 2022 NEJM article documented cases of multifocal pneumonia in leukemia patients where fungal causes were initially missed due to lack of fever or sputum production—highlighting the importance of high clinical suspicion.
Treatment Considerations:
- Broad-spectrum antibiotics + antifungals or antivirals early
- Regular imaging for surveillance
- Use of prophylactic antimicrobials in transplant protocols
Pregnancy and Multifocal Pneumonia
Though rare, multifocal pneumonia in pregnancy can pose risks to both mother and fetus.
Key Concerns:
- Reduced lung capacity in late pregnancy makes respiratory distress more dangerous.
- Limited medication options due to fetal safety.
- Higher risk of complications with influenza or COVID-19.
Management Includes:
- Early antiviral use (if viral etiology suspected)
- Safe antibiotics (e.g., ceftriaxone, azithromycin)
- Supplemental oxygen to maintain fetal oxygenation
Guideline Note: The American College of Obstetricians and Gynecologists (ACOG) recommends hospital admission for pregnant women with suspected multifocal pneumonia, especially if O₂ saturation falls below 95%.
Answer Engine Optimization FAQs
How does multifocal pneumonia affect the elderly?
Older adults may have unusual symptoms like confusion, and are at higher risk of severe illness, hospitalization, and death.
Is multifocal pneumonia dangerous for babies?
Yes. It can progress quickly, especially in infants under 6 months. Prompt medical attention is crucial.
Can immunocompromised patients recover from multifocal pneumonia?
Yes, but they often need aggressive, specialized treatment including antifungals or antivirals and longer recovery times.
Potential Complications of Multifocal Pneumonia
Multifocal pneumonia is more than just a lung infection. Because it involves multiple regions of the lungs, it carries a higher risk of severe complications compared to localized pneumonia—especially when treatment is delayed or the patient is already vulnerable due to age or chronic illness.
Understanding these complications is essential for clinicians, caregivers, and patients alike to monitor symptoms, act quickly, and prevent long-term damage.
1. Respiratory Failure
This is one of the most serious and immediate risks of multifocal pneumonia.
When the infection spreads across several lung regions, the lungs struggle to perform gas exchange, resulting in low oxygen levels (hypoxemia) or buildup of carbon dioxide (hypercapnia).
Signs of Respiratory Failure:
- Oxygen saturation < 90%
- Gasping for breath
- Bluish lips or fingertips (cyanosis)
- Confusion or inability to stay awake
Patients may require:
- High-flow oxygen
- Non-invasive ventilation (BiPAP or CPAP)
- Mechanical ventilation (intubation) in critical cases
Clinical Data: In a 2023 multi-center ICU study (Critical Care Medicine), 48% of patients with multifocal pneumonia required intubation, with an average ventilation time of 9 days.
2. Acute Respiratory Distress Syndrome (ARDS)
ARDS is a life-threatening inflammatory lung condition that can be triggered by multifocal pneumonia, especially when caused by viruses like COVID-19 or influenza.
What Happens in ARDS:
- Alveoli (air sacs) fill with fluid
- Lungs stiffen, making breathing extremely difficult
- Oxygen delivery to the bloodstream drops dramatically
Risk Factors for ARDS:
- Delayed treatment
- High viral load
- Immunosuppression or pre-existing lung disease
Treatment typically requires ICU care, mechanical ventilation, and sometimes prone positioning (lying the patient face-down) to improve oxygenation.
3. Sepsis and Septic Shock
Multifocal pneumonia can allow bacteria or inflammatory markers to enter the bloodstream, triggering sepsis—a body-wide, life-threatening response to infection.
Signs of Sepsis:
- High or dangerously low body temperature
- Rapid heart rate and breathing
- Confusion or disorientation
- Very low blood pressure (septic shock)
Treatment:
- Immediate IV antibiotics
- IV fluids and vasopressors to maintain blood pressure
- Organ support (e.g., dialysis if kidneys fail)
Fast Fact: According to the Sepsis Alliance, 1 in 3 hospital deaths is related to sepsis, and pneumonia is a top cause.
4. Lung Abscess
A lung abscess is a localized pocket of pus that forms inside the lung when tissue is destroyed by the infection.
Clues on Imaging:
- Cavitary lesion with air-fluid level
- Often in gravity-dependent regions of the lung
Treatment:
- Prolonged course of IV antibiotics
- Drainage via needle aspiration or surgery if the abscess is large
Lung abscesses are more common in aspiration pneumonia, alcoholics, and patients with poor oral hygiene.
5. Pleural Effusion and Empyema
The infection can spread to the pleural space (the area between the lungs and chest wall), causing fluid buildup—called a pleural effusion. When this fluid becomes infected, it turns into empyema.
Diagnosis:
- Chest ultrasound or CT
- Thoracentesis (fluid analysis)
Treatment:
- Drainage with a chest tube
- Antibiotics
- Sometimes surgery (VATS or open decortication)
Empyema significantly prolongs hospital stays and can delay full recovery.
6. Chronic Respiratory Issues and Lung Scarring
Even after the acute infection resolves, some patients are left with long-term lung damage—especially those who experienced severe multifocal pneumonia or required mechanical ventilation.
Long-Term Effects Can Include:
- Fibrosis (scarring) in affected lung areas
- Decreased lung capacity
- Persistent shortness of breath
- Increased risk of future infections
Pulmonary rehabilitation, breathing exercises, and regular follow-ups with a pulmonologist may be needed for months after recovery.
Answer Engine Optimization FAQs
Can multifocal pneumonia be fatal?
Yes. If not treated promptly, multifocal pneumonia can lead to life-threatening complications such as respiratory failure, sepsis, or ARDS. Early medical intervention greatly reduces the risk of death.
How long does it take to recover from multifocal pneumonia?
Recovery time varies. Mild cases may resolve in 1–2 weeks, while severe or hospitalized cases can take 4–8 weeks or more. Some patients may have lingering symptoms for several months.
What is the difference between pneumonia and multifocal pneumonia?
While pneumonia affects a single part or lobe of the lung, multifocal pneumonia involves multiple regions of one or both lungs. This makes it more severe and often harder to treat.
Can you prevent multifocal pneumonia?
Yes. Vaccinations (like pneumococcal, flu, and COVID-19 vaccines), hand hygiene, and avoiding smoking are all effective preventive measures—especially in high-risk groups.
What are signs that multifocal pneumonia is getting worse?
Red flags include:
- Increasing shortness of breath
- Confusion or fatigue
- Persistent high fever
- Blue lips or extremities
- Oxygen levels dropping below 92%
Seek emergency care if any of these symptoms occur.
Is multifocal pneumonia contagious?
The underlying infection (like a virus or bacteria) may be contagious, but pneumonia itself is not. Good hygiene and isolation when sick can reduce transmission risk.
Conclusion: Understanding and Managing Multifocal Pneumonia
Multifocal pneumonia is a serious respiratory condition that demands timely diagnosis, personalized treatment, and close monitoring—especially for the elderly, children, and immunocompromised individuals. Its defining feature—involvement of multiple areas of the lungs—makes it more complex than standard pneumonia and potentially more dangerous.
Thanks to advancements in imaging, antibiotics, antivirals, and critical care, most patients can recover fully, especially when treatment begins early. However, post-recovery care, including pulmonary rehab and routine follow-ups, is often necessary for long-term healing.
Here’s a quick recap:
- Early detection and treatment save lives
- CT scans and lab tests are crucial for diagnosis
- Hospitalization may be required for moderate to severe cases
- Complications like ARDS or sepsis must be anticipated and prevented
- Prevention through vaccination and hygiene remains the most effective strategy
Whether you’re a patient, caregiver, or clinician, staying informed about multifocal pneumonia can make the difference between a routine recovery and a medical emergency.
“The lungs are precious—take care of them before you need to rely on machines to do what breath once did effortlessly.”
